Overjet
Founded Year
2018Stage
Series C | AliveTotal Raised
$130.55MValuation
$0000Last Raised
$53.2M | 1 yr agoMosaic Score The Mosaic Score is an algorithm that measures the overall financial health and market potential of private companies.
+29 points in the past 30 days
About Overjet
Overjet focuses on dental artificial intelligence (AI) and operates within the healthcare technology sector. It offers a platform that supports dental providers and payers by enhancing clinical care and administrative efficiency through AI-driven radiographic analysis and claims processing optimization. The company primarily sells to the dental industry, including dental service organizations (DSOs), dental groups, and insurance companies. It was founded in 2018 and is based in Boston, Massachusetts.
Loading...
Overjet's Product Videos
_OnePager_v2_thumbnail.png?w=3840)
ESPs containing Overjet
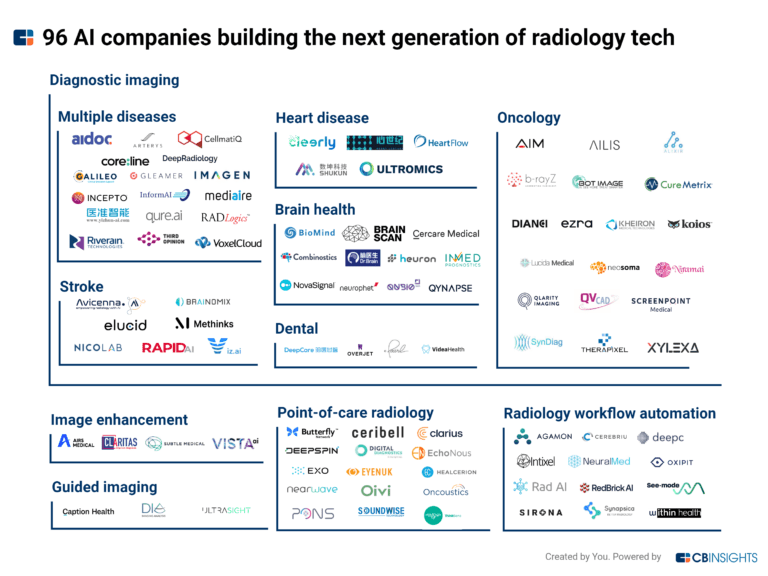
The ESP matrix leverages data and analyst insight to identify and rank leading companies in a given technology landscape.
The dental imaging analytics platforms market aims to improve the accuracy and efficiency of dental disease detection and treatment. Vendors here are using tech to detect and diagnose dental conditions such as cavities, gum disease, and oral cancer by analyzing X-ray and 3D imaging data. Tech is also used to detect early signs of periodontal disease and identify the presence of impacted teeth. The…
Overjet named as Leader among 9 other companies, including Philips, Pearl, and VideaHealth.
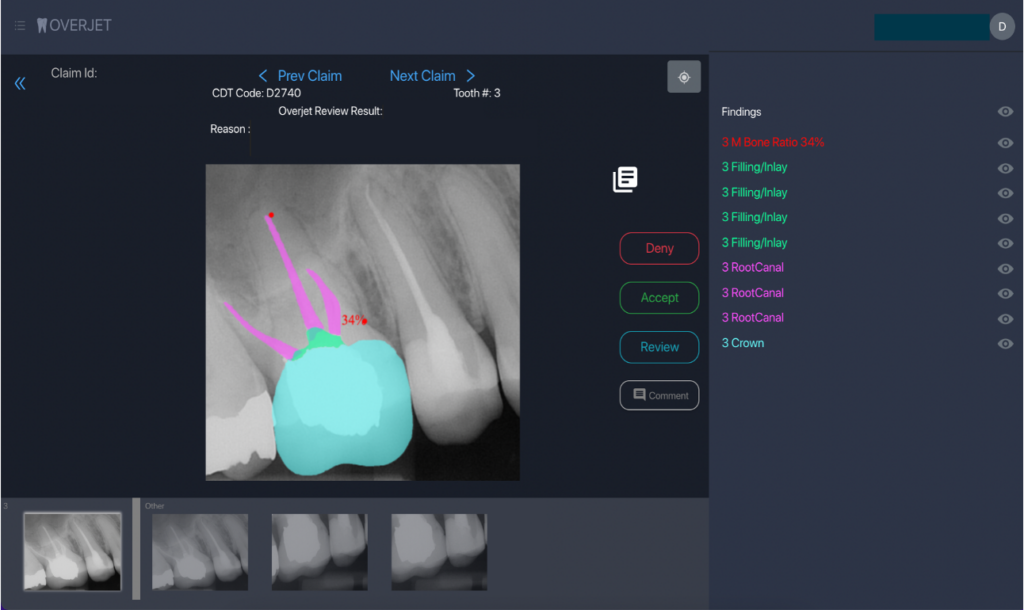
Overjet's Products & Differentiators
Insurance Intelligence Platform
The Insurance Intelligence Platform is the only end-to-end utilization review solution that can make expert, compliant decisions on dental insurance claims — using a powerful combination of AI and independent, licensed reviewers.
Loading...
Research containing Overjet
Get data-driven expert analysis from the CB Insights Intelligence Unit.
CB Insights Intelligence Analysts have mentioned Overjet in 4 CB Insights research briefs, most recently on May 16, 2025.
May 16, 2025 report
Book of Scouting Reports: 2025’s AI 100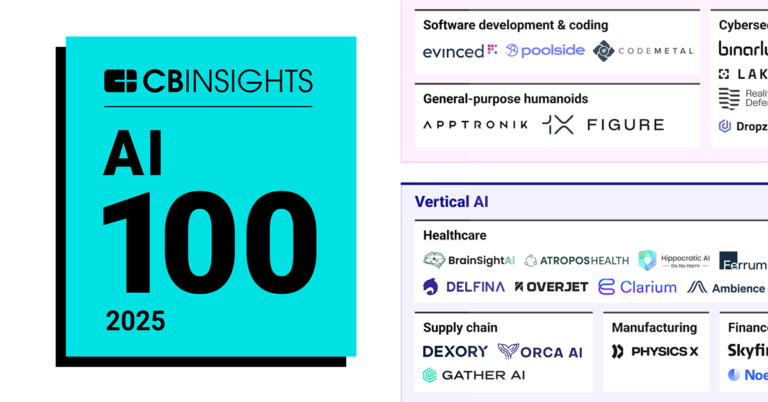
Apr 24, 2025 report
AI 100: The most promising artificial intelligence startups of 2025Expert Collections containing Overjet
Expert Collections are analyst-curated lists that highlight the companies you need to know in the most important technology spaces.
Overjet is included in 9 Expert Collections, including Insurtech.
Insurtech
3,347 items
Companies and startups that use technology to improve core and ancillary insurance operations. Companies in this collection are creating new product architectures, improving underwriting models, accelerating claims and creating a better customer experience
Fintech
9,653 items
Companies and startups in this collection provide technology to streamline, improve, and transform financial services, products, and operations for individuals and businesses.
Digital Health
11,408 items
The digital health collection includes vendors developing software, platforms, sensor & robotic hardware, health data infrastructure, and tech-enabled services in healthcare. The list excludes pureplay pharma/biopharma, sequencing instruments, gene editing, and assistive tech.
AI 100 (All Winners 2018-2025)
200 items
Winners of CB Insights' 5th annual AI 100, a list of the 100 most promising private AI companies in the world.
Digital Health 50
300 items
The winners of the third annual CB Insights Digital Health 150.
Insurtech 50 (2024)
50 items
Report: https://www.cbinsights.com/research/report/top-insurtech-startups-2024/
Overjet Patents
Overjet has filed 6 patents.
The 3 most popular patent topics include:
- image processing
- medical imaging
- dentistry

Application Date | Grant Date | Title | Related Topics | Status |
|---|---|---|---|---|
12/22/2021 | 12/3/2024 | Dentistry, Artificial neural networks, Optical illusions, Acquired tooth disorders, Dental materials | Grant |
Application Date | 12/22/2021 |
|---|---|
Grant Date | 12/3/2024 |
Title | |
Related Topics | Dentistry, Artificial neural networks, Optical illusions, Acquired tooth disorders, Dental materials |
Status | Grant |
Latest Overjet News
Jul 1, 2025
Subjects Abstract This research introduces Oral Score Basic (OS-B), a novel Artificial Intelligence (AI) derived methodology designed to provide a comprehensive, objective assessment of individual teeth and overall oral health, initially focused on dental conditions. Leveraging data from more than 340,000 patients across 2,558 U.S. dental practices, OS-B combines radiographic findings and periodontal probing depths with a treatment probability-weighted cost function to quantify the severity of dental conditions. The OS-B score aims to address limitations in prior oral health scoring systems by incorporating nuanced clinical data accounting for disease severity, and providing a scalable, data-driven approach to measuring oral health. This score was developed using Overjet’s FDA-cleared AI platform, which detects dental conditions using bitewing and periapical radiographs, providing a detailed analysis of each tooth. OS-B’s effectiveness was validated by demonstrating a strong correlation between tooth scores and treatment costs, surpassing the predictive power of previous scoring systems. This research presents a foundational framework for AI-enabled oral health scoring, with potential applications in value-based care, population risk analysis, and consumer health management. Future iterations may expand to include additional dimensions of oral health beyond clinical conditions such as risk factors and measures of oral function and esthetics, further enhancing the score’s public health and clinical utility and patient engagement. Introduction Oral health is a critical component of overall health and well-being; yet quantifying it comprehensively has remained a challenge. Over the past five decades, numerous oral health scores have been developed to summarize oral health status and to measure the impact of healthcare interventions. Notable examples include the work of Nikkias et al. 1 , 2 , the Index of Oral Health Status by Marcus et al. 3 , the Oral Health Index published by Burke and Wilson 4 that was later modified and developed by Denplan (Winchester, UK) and renamed the Oral Health Score 5 . Self-reported measures of oral health and oral health related quality of life such as the OHIP-5 6 , and the GOHAI 7 have been developed and extensively validated. However, these measures are based on patient reports and have several important limitations including recall bias, lack of clinical specificity, and limited sensitivity to change following treatment interventions. More recently, commercial products such as Previser have emerged as an evidence-based risk score for oral diseases 8 . While these previous efforts have been valuable, they are constrained by limited sample sizes and often rely on binary disease classifications, failing to capture the nuanced complexity of oral health conditions. The advent of artificial intelligence (AI) and advanced computer vision techniques powered by deep learning now presents an unprecedented opportunity to revolutionize oral health assessment. Table 1 provides a comparative overview of prior methodologies to create an oral health outcome measure, highlighting both their strengths and limitations in relation to a new proposed methodology that utilizes AI derived clinical findings and cost-weighting in a large U.S. national data set (OS-B). While existing tools like the Oral Health Status Index (OHSI), the 5-item Oral Health Impact Profile (OHIP-5), and traditional epidemiological measures—such as the Decayed, Missing, and Filled Teeth (DMFT) index and the Community Periodontal Index (CPI)—serve specific purposes, they do not offer a comprehensive measure of oral health status or effectively predict treatment needs and related costs. These indices typically rely on subjective evaluations, whereas the proposed OS-B leverages AI-driven detection and a treatment probability-weighted cost function, resulting in a more precise and clinically relevant evaluation. Table 1 Comparative overview of oral health indices: strengths, limitations, and performance relative to the proposed ai enabled composite oral score. The development of a more sophisticated oral health score is imperative, driven by several significant healthcare trends. The ongoing transformation from fee-for-service to value-based care models necessitates robust outcome measures. An AI-derived oral health score could precisely quantify changes in oral health related to clinical interventions, enabling more accurate assessment of care effectiveness. Concurrently, the shift in dental practice modality, with an increasing rate of dentists affiliating with dental support organizations and practicing in groups 9 , provides an opportunity to measure and monitor services provided and their impact on health status. Moreover, the growing consumer interest in health monitoring and management calls for accessible tools that empower individuals. A consumer-friendly oral health score could play a crucial role in early detection and prevention, potentially reducing the need for invasive and costly treatments. Gamification of such a score could further engage and motivate consumers to better manage their oral health. Finally, private or public payers of care would benefit from an objective clinical outcome measure that could be utilized in population risk analysis, plan design, and provider network assessment. These factors collectively underscore the need for a comprehensive, AI-driven oral health score that can serve multiple stakeholders in the healthcare ecosystem. This research aims to address these needs by developing and validating a novel, AI-enabled composite oral score—Oral Score Basic (OS-B)—that overcomes the limitations of prior oral health scoring systems. Our methodology leverages large-scale clinical data from 2558 dental practices and more than 343,000 patients across all 50 U.S. states, representing one of the most comprehensive and geographically diverse datasets ever used in dental research. OS-B uses objective, quantifiable measures to assess individual tooth health, combining radiographic findings and periodontal measurements with a treatment probability-weighted cost function. This approach moves beyond binary disease classification by capturing disease severity—for example, quantifying caries using the relationship between DMFP and treatment cost. Tooth-level scores are generated using FDA-cleared deep learning models, which provide consistent and scalable assessments far more reliable than self-reported or examiner-dependent evaluations. The individual tooth scores are then averaged to compute a patient-level oral score. Because this initial version focuses specifically on dental health indicators, we refer to it as Oral Score – Basic (OS-B). This foundational research establishes a framework that can be expanded to include additional oral health dimensions such as function, esthetics, and patient-reported outcomes, aligning with the World Health Organization’s holistic definition of oral health 10 .We hypothesize that AI-driven analysis can yield a more consistent, objective, and scalable approach to oral scoring based on the most comprehensive and accurate data available and tested this hypothesis by comparing the OS-B scores to the Marcus et. Al OHSI 3 . Our study utilizes AI analysis of dental radiographs from an unprecedented sample of 343,297 patients across 2,558 dental practices in the United States. This extensive dataset allows for a more nuanced and comprehensive assessment of dental conditions than ever before possible. By developing this innovative scoring system, we aim to provide a valuable tool for clinicians, researchers, and policymakers to better understand, monitor, and improve oral health outcomes. Additionally, with further development and validation, the OS-B has the potential to empower consumers in managing their oral health, ultimately contributing to improved overall health and reduced healthcare costs. Methods The OS-B is built using data from 2,558 dental practices across the United States who used the Overjet, Inc. Practice Application 11 and includes data from 321,530 adult patients who were 21 years of age or older (Figure 1 ). All patient data were deidentified in accordance with HIPAA guidelines to ensure confidentiality. These practices are located in every U.S. state as well as Puerto Rico. Fig. 1 The development of the OS-B included defining the clinical components of the score, developing a test dataset and subsets, and developing a novel treatment probability weighted cost-function to calculate a weighted individual tooth score from each of the patient’s 28 permanent teeth, excluding third molars. The adult human dentition typically includes up to 32 teeth, including four third molars (wisdom teeth). Contemporary dental public health research increasingly adopts 28-tooth frameworks for population-level studies. This methodology uses the 28 tooth framework in order to determine a more consistent and comparable metric across diverse demographic groups, minimizing confounding variables associated with third molar variability. We acknowledge that third-molars can impact overall health, particularly in the context of periodontal disease, and future research should further explore the use of the 32- vs. the 28-tooth framework in the score calculation. For the purposes of this study, individual tooth scores for the patient’s 28 permanent teeth were then averaged into a mouth-level summary score called OS-B. Once constructed, we conducted a preliminary validation of OS-B on the test dataset and compared the OS-B to the Marcus et. al OHSI 3 . The clinical condition of the 28 permanent teeth was assessed using findings from the Overjet AI platform and its proprietary, FDA-cleared Machine Learning Algorithms (MLA) along with periodontal probing depth data from patient electronic records. Overjet’s AI models for detecting and segmenting caries, calculus, periapical radiolucencies (PARL), margin discrepancies, and existing restorations—including fillings, crowns, root canal-treated (RCT) teeth, and implants—are all based on a proprietary Convolutional Neural Network architecture designed to perform object detection and segmentation on dental radiographs. The architecture includes a CNN backbone based on ResNet with Feature Pyramid Network (FPN) for feature extraction, a Region Proposal Network (RPN) to generate candidate object regions, and a final stage that predicts bounding box locations, instance masks, and keypoints as needed. Table 2 presents the standalone sensitivity and specificity of each model used in this research. Table 2 Standalone sensitivity and specificity of Overjet’s AI models for dental condition detection and segmentation. (3) The type and extent of dental restorations on an individual tooth including radiographic evidence of full and partial coverage crowns, fillings, root canals, and/or the presence of a dental implant in place of the tooth. (4) The percentage of the tooth’s coronal tooth structure that is decayed, missing and/or filled, calculated by the Overjet platform as the Decayed, Missing, and/or Filled Proportion (DMFP). (5) Interproximal alveolar bone levels (ABL) measured in millimeters from the cemento-enamel junction (CEJ) to the most apical crest of the interproximal alveolar bone, as an indicator of the tooth’s periodontal status. (6) Interproximal calculus on cementum for each tooth on both bitewing and periapical radiographs, scored as either absent or present. (7) Periapical Radiolucencies (PARL) on periapical radiographs that may or may not be associated with an endodontic root filling. PARL is scored as either absent or present. (8) Margin discrepancy (MD) where a full or partial coverage crown or filling has a defective margin, an over contoured or under contoured restoration, or an overhang where a restorative material extends beyond or over the margin apically. MD is scored as either absent or present. Note that this feature of the Overjet AI platform is not currently FDA cleared but was included in the analysis because it adds information about the quality of existing restorations. AI model performance and training process As part of the data cleaning and preprocessing pipeline, all patient and clinic data extracted from practice management systems (PMS) were assigned unique identifiers to prevent cross-association of information. Radiographs were matched to appointment dates, and any radiographs lacking an associated appointment date, as well as patients without documented age, were excluded from the dataset. Additionally, data related to proposed dental treatment plans or delivered treatments were linked to the corresponding patient and appointment using unique identifiers to ensure data consistency and integrity across clinical records. These steps were implemented to ensure that only accurate, complete, and temporally consistent data were used in developing and validating the OS-B score. The AI models utilized in this study were originally developed and trained for clinical applications, using a robust dataset that reflected diversity across key variables such as patient demographics, image quality, and sensor types. Radiographs were annotated by calibrated dentists trained through a standardized internal process. While the models were not trained specifically for this research, they were applied here in the context of oral health quantification, demonstrating adaptability to new use cases beyond their original clinical deployment. We implemented a methodical data partitioning strategy, creating separate training and test sets with the test set comprising tens of thousands of radiographs. Both datasets maintained balanced distributions across demographic and imaging characteristics. To ensure unbiased performance evaluation, we enforced strict patient-level separation between training and test sets, preventing any single patient’s data from appearing in both. Our development follows a continuous improvement methodology based on real-world performance feedback. We systematically monitor model performance in clinical deployment settings and analyze practitioner feedback to identify specific failure patterns or edge cases. This intelligence informs our dataset enrichment strategy, allowing us to augment both training and test datasets with representative examples of challenging scenarios. This feedback loop enables our models to progressively improve their generalization capabilities, particularly for clinically important but statistically underrepresented presentations. Developing the dataset For the purposes of this study, we used deidentified data from 2,558 dental practices, which were randomly divided into three categories: a training dataset (n = 1,808), a validation dataset (n = 254) and a test dataset (n = 496). The training dataset was further subdivided to calculate a treatment probability-weighted cost-function for four clinical conditions: (1) (4) Periapical radiolucency. For each patient in the training dataset, we included clinical findings from their most recent dental radiographs, along with treatments provided in the 12 months following the latest radiographs as documented in the patient record using CDT codes. The average cost associated with each CDT code was calculated across all clinics. Additionally, probing depth (PD) measurements for each tooth were extracted from the patient records, with the maximum probing depth per tooth serving as an indicator of periodontal status. Each data subset was constructed by applying filtering criteria. Initially, Overjet’s MLA determined the teeth as positive for specific findings and negative for others. Subsequently, the teeth were required to have received a specified set of treatments within one year of detecting a clinical finding being detected on a radiograph, as documented by CDT codes extracted from the patient records. Any treatments provided outside the primary dental practice were not available for inclusion in the dataset. Table 3 provides an overview of the patient count, tooth count, along with the inclusion and exclusion criteria for the overall training dataset and subsets. For example, the caries subset includes teeth identified by Overjet’s MLA as positive for caries and negative for other clinical findings, such as margin discrepancies, calculus, root tips, bone levels exceeding 2.0 mm, PARL, implants, crowns, root tips, and bridges. Additionally, each tooth was required to have received treatment – such as a filling, crown, root canal therapy (RCT), extraction, or implant – within one year from the time of detection, as indicated by CDT codes in the patient’s electronic record, to remain in the dataset. These filtering criteria ensured that teeth included in each dataset were treated primarily due to conditions detected by Overjet AI. Table 3 The number of patients, number of teeth, inclusion and exclusion criteria for the training data set and each data subset for the four specific clinical conditions. The inclusion and exclusion criteria in Table 3 were designed to isolate the impact of each clinical condition on treatment decisions. For each condition, criteria were selected to ensure that the treatment received was most likely attributable to that specific finding, minimizing confounding effects from co-occurring conditions. For example, in the caries subset, teeth with other significant findings—such as PARL, crowns, implants, RCTs, bridges, or alveolar bone levels greater than 2 mm—were excluded to ensure that the treatment was primarily due to caries alone. Similarly, for the PARL subset, teeth were included only if they were positive for PARL and free from other overlapping conditions that could independently influence treatment. This approach was the most effective way to reduce confounding effects when attributing treatment patterns and costs to individual clinical findings. Table 4 summarizes patient age and gender distribution across the overall training dataset and within each data subset for the four specific clinical conditions. Patients within the caries subset were slightly younger than those in the overall training dataset. In contrast, patients with the remaining clinical conditions were older, on average, which aligns with the increased prevalence of these conditions with advancing age. Table 4 Summary of patient age (median, mean, standard deviation) and gender distribution for the overall training dataset and subsets defined by four specific clinical conditions. Development of a “treatment probability weighted cost-function” to calculate the OS-B tooth scores This research uses multiple data inputs to derive a novel treatment probability-weighted cost function for determining an individual tooth score. Using tooth-specific treatments administered within 12 months after the dental radiographs and the tooth’s state as calculated by Overjet’s MLA, we developed a function to estimate treatment costs based on the tooth’s clinical condition. The tooth score is based on the treatment cost needed to restore the tooth. The scoring acknowledges that dental restorations cannot perfectly replicate original tooth health. Higher treatment costs correspond to a lower tooth score, and lower costs correspond to a higher score. Once the individual tooth scores are calculated, the patient’s OS-B is determined by averaging the tooth scores of 28 individual teeth, excluding third molars. The treatment probability-weighted cost function integrates both the likelihood and cost of various dental treatments indicated for specific clinical conditions. The clinical state of the tooth determines a distribution of possible treatments. The estimated treatment cost is calculated by multiplying the cost of each treatment by its associated probability. Finally, this expected treatment cost is used to adjust the tooth’s health score by subtracting the weighted cost from the base score of 100 (representing a healthy tooth). A score of 100 is assigned to a healthy tooth that exhibits no restorations or pathology. As clinical findings are detected, the score decreases accordingly. For example, a tooth exhibiting initial caries or radiolucent areas of demineralization would have a higher score than a tooth with more extensive caries requiring more invasive and expensive treatment. Conversely, a tooth with extensive caries is assigned a lower score due to the likelihood of needing a multi-surface or full coverage restoration to return it to a state of health. To illustrate how a tooth is scored using the treatment probability-weighted cost-function, we initially focused on the caries data subset, employing the DMFP as a metric for coronal caries severity. Within our training dataset, caries emerged as the most common clinical finding, affecting 85.2% of patients and 67.3% of teeth. Figure 4 A and B plot the probability of treatment and treatment cost against the DMFP value of a tooth with caries, respectively, and Fig. 4 C plots tooth score as a function of DMFP. At low DMFP, the treatment cost is relatively low because only a small proportion of coronal tooth structure is compromised by demineralization or caries and a dental restoration or filling is the most performed treatment. As the DMFP increases treatment cost increases, as a larger portion of the tooth is compromised, necessitating more extensive interventions such as crowns, root canals, or extraction and placement of implants. These treatments are more invasive and expensive, leading to higher overall treatment costs. Fig. 4 (A) Treatment distribution across DMFP values. The red line represents the probability of receiving a filling, which steadily declines as DMFP increases. As the DMFP value increases, the likelihood of more extensive treatments increases; the orange line shows the probability of crown placement, which peaks at a DMFP value of approximately 0.68 before declining. The green line indicates the probability of root canal therapy (RCT), which rises with DMFP. The blue line represents the combined probability of extraction or implant placement, which increases sharply with higher DMFP scores. These trends mirror clinical practice, where increasing structural damage drives a shift toward more invasive and costly interventions. The error bars in this panel illustrate the 95% confidence intervals of the computed probabilities. (B) Treatment cost as a function of DMFP. This plot illustrates how treatment costs escalate with increasing DMFP. The red line depicts the average observed cost of treatment within 12 months following the assessment, which increases with rising DMFP values, reflecting the need for more extensive and expensive procedures as disease severity worsens. The green line represents a second-degree polynomial approximation of cost, which closely aligns with the observed trend, validating the reliability of the prediction. (C) Tooth score and caries-related deductions across DMFP values. This panel displays how the OS-B score for a tooth is calculated based on its DMFP. The blue line shows the resulting tooth score, which declines from 100 to 0 as DMFP increases from 0 to 1. In contrast, the green line shows the number of points deducted due to caries, which rises proportionally with DMFP. The deduction is derived by linearly scaling the cost function in (B), such that no points are deducted when DMFP is 0 and the maximum 100-point deduction is applied when DMFP is 1. The opposing trajectories of the two lines highlight the scoring logic and the increasing impact of carious damage. Treatment patterns in Fig. 4 A reflect clinical treatment distributions based on DMFP values. When DMFP is low—indicating minimal damage to tooth structure—fillings are the predominant treatment choice, allowing for conservative management of demineralized and carious tooth structure. As DMFP increases, showing greater structural compromise of the coronal tooth structure, treatments shift toward more extensive options like crowns, root canal therapy (RCT), or extractions with implant placement. This progression mirrors clinical practice, where severely damaged teeth require more extensive rehabilitation. DMFP, while a valuable indicator of structural damage, is just one factor considered when making clinical treatment decisions. Clinical care is also influenced by dentist preferences, patient choices, symptoms, overall health, medical history, insurance coverage, and socioeconomic factors. For example, a patient with a high-DMFP tooth might choose extraction over a crown, RCT, or implant due to cost concerns, limited insurance, or access barriers to more complex and often more expensive treatment. This likely explains the sharp increase in extraction probability at higher DMFP values. While these external factors introduce variability in treatment selection, particularly in moderate to severe cases, the overall treatment trends consistently reflect how damage of the coronal tooth structure guides clinical decision-making in dental practice. Figure 4 B illustrates the relationship between a tooth’s DMFP and its treatment cost for the next 12 months. We approximate this relationship using a second-degree polynomial of the form (green curve in Figure 4 B). $$Cost = a*DMFP + b*{DMFP}^{2}$$ Values of a and b are obtained using the least squares regression algorithm. The tooth score is calculated by subtracting points from 100, with the deduction proportional to treatment costs over the next 12 months. This is mathematically realized by linearly scaling the polynomial via the following 2 constraints: no points are deducted when the DMFP is 0, and 100 points are deducted when the DMFP = 1. Figure 5 A illustrates the variation in treatment costs as a function of DMFP. At lower DMFP values, indicating less compromised coronal tooth structure, fillings are the most common treatment, with costs ranging from $200 to $600. As DMFP increases, the likelihood of full-coverage restorations (crowns) and extractions followed by dental implant placements, also increases, resulting in higher associated costs, as shown in Figure 5 B. Consequently, the cost distribution shifts upward, and for DMFP values exceeding 0.8, extraction and implant placement become the most likely treatment, with typical costs ranging from $3000 to $4000. Fig. 5 (A) Treatment cost distribution as a function of DMFP in the caries dataset. At each DMFP interval, the minimum, maximum and mean costs are indicated by markers ( −) at the bottom, middle, and top of each vertical bar, respectively. The blue violin plots represent the density of treatment costs, indicating the intervals where treatment costs are most frequently observed. (B) Stacked bar chart showing treatment probabilities across the same DMFP intervals. As DMFP increases, the likelihood of more complex treatments (crown, RCT, extraction + implant) increases, while the probability of receiving a filling decreases. A tooth’s score after restoration depends on two factors: the severity of the decay and compromised coronal tooth structure and the understanding that dental treatments cannot fully restore a tooth to perfect health. Our research estimates that restored teeth regain approximately 80% of their original health status. The severity is measured by the tooth’s Average DMFP which is defined as $${DMFP}_{average}=\frac{{\sum }_{DMFP=0}^{1.0}P(treatment | DMFP)* DMFP}{P(treatment) }$$ Here \(P(treatment | DMFP)\) denotes the probability of treatment for a given DMFP, derived from Fig. 5 B. For example, the average DMFP for a crown treatment is 0.59. A tooth with this level of decay loses 50 points from its score. After crown placement, the tooth recovers 80% of these lost points, meaning only 10 points (20% of 50) are permanently deducted. This scoring system reflects that while restorative treatments significantly improve tooth function, they cannot achieve the same level of health as an original, undamaged tooth. Table 5 includes the determination of weightings for four types of restorations: 1) a full coverage restoration (crown); 2) a root canal treatment; 3) filling; and 4) an extraction and placement of a dental implant. Table 5 Determination of weightings various restorations based on the tooth’s DMFP. The number of points deducted for a filling depends on its size, with a minimum deduction of 4.6 points and a maximum of 10 points. Here we capped the point deductions for fillings to that of a crown treatment because filling treatments generally retain more original coronal tooth structure as compared to a crown. To account for findings such as PARL and recurrent caries under crowns, we used a simple weighted average technique to determine point deductions. For each of these conditions we obtained the probability distribution of different treatment types, and used the DMFP-based point deduction for each of those treatments together with the probabilities as the weights, to find the average point deductions. Table 6 provides a summary of the treatment distributions and corresponding point deductions for PARL and recurrent caries under crown restorations, as represented by the following formula: $${TS}_{condition}= \sum\limits_{t=1}^{n}P(t){TS}_{t}$$ where \({TS}_{condition}\) represents either PARL or recurrent caries under crown, \(P(t)\) denotes the probability of a given treatment for the condition, and \({TS}_{t}\) is the DMFP-based point deduction for the treatment performed for the condition. Table 6 Summary of treatment distribution and tooth score point deductions for PARL and recurrent caries associated with a crown restoration. Points are deducted when a tooth’s bone levels exceed 2.0 mm, where a measurement ≤ 2.0 mm is considered healthy. The deduction amount is proportional to the treatment cost at that bone level. Figures 6 A and B illustrate the treatment probability and associated costs over the next 12 months as a function of a tooth’s bone level. Fig. 6 (A) Probability of various treatment types based on the bone level of teeth in the AL & PD dataset. The error bars in this panel illustrate the 95% confidence intervals of the computed probabilities. Advanced treatments may include procedures such as gingival flap surgery, osseous surgery, bone replacement grafts, and distal or proximal wedge procedures. (B) Relationship between treatment cost and bone level for the same set of teeth. The blue curve represents the estimated treatment costs, while the red line shows a first-degree polynomial approximation of cost. (C) Tooth Score vs. Bone Level. Tooth score decreases linearly as bone level exceeds 2.0 mm, with deductions scaled to treatment cost (B). At 6.71 mm, the average extraction threshold, 63.5 points are deducted. This scoring approach aligns with caries-based indices for consistent assessment of tooth health. $$Cost = a*BL + b$$ The values of \(a\) and \(b\) are determined using the least squares regression algorithm. This first-order polynomial is then linearly scaled based on two constraints: no points are deducted when the bone level is less than or equal to 2.0 mm, and 63.5 points are deducted when the bone level reaches 6.71 mm. Similar to the Average DMFP, the Average Bone Level (\(BL\)) for extraction is 6.71 mm. We propose that the tooth score for a tooth requiring implant placement and restoration whether due to elevated bone levels or severe caries, should be equivalent. Figure 6 C plots tooth score as a function of bone level. Interproximal calculus on a tooth’s cementum typically requires scaling and root planing (SRP) treatment, with an associated cost equal to that of a tooth displaying a DMFP of 0.07, as seen in Figure 4 B. According to the relationship between DMFP and tooth score (Figure 4 C), 4.5 points are deducted from a score of 100 at this DMFP. Therefore, the presence of interproximal calculus results in a 4.5-point deduction. Similarly, a tooth typically requires SRP treatment when its probing depth exceeds 4 mm. Following the same point deduction approach as for interproximal calculus, 4.5 points are deducted when the probing depth surpasses 4 mm. Point deductions due to Margin Discrepancy (MD) vary based on its type. If the margin discrepancy occurs on a filling, the deduction is based on the tooth’s DMFP. If the MD occurs on a crown, we assume that the tooth requires crown replacement, leading to a deduction of 50 points. A deduction of 100 points is applied when a tooth is missing or when only a root tip remains. Table 7 summarizes the point deductions for each clinical condition. Table 7 Summary of point deductions for each clinical condition. The previous sections explored how each of the eight clinical findings affects individual tooth scores. Each individual finding results in a specific number of points deducted from an ideal score of 100. When multiple findings are present, each deduction is calculated separately and then they are combined, as illustrated in Figure 7 . The total deduction is subtracted from 100 to yield the final tooth score, while missing teeth and root tips are automatically assigned a score of zero. Fig. 7 OS-B is calculated by first determining individual tooth scores, as shown in this figure, and then averaging these scores across the 28 permanent teeth, excluding third molars. Missing teeth and root tips are assigned a score of zero. Since multiple conditions can often be addressed with a single restorative or endodontic procedure, treatment costs are non-additive. Thus, deductions for decay, MD, and PARL are combined by taking the maximum value among these findings. Similarly, deductions for elevated probing depth and interproximal calculus are also combined using the maximum value, as both conditions are typically treated together through SRP. Bone level deductions are treated independently from other findings, reflecting their distinct nature and specific treatment requirements. Restorative deductions (crowns and fillings) are only applied if there is no concurrent MD or decay, as restorations are automatically accounted for by the DMFP when these conditions are present. Figure 7 provides an illustration of the calculation process for individual tooth scores, while Figures 8 and 9 demonstrate the application of these calculations in patient cases. Fig. 8 Patient A’s original full-mouth X-rays (FMX) without AI predictions can be compared to the AI-analyzed FMX. Using AI predictions and the calculated oral score for each tooth, the odontogram provides individual tooth scores and an overall oral score. Patient A has an overall Oral Score of 65.5, impacted by findings including PARLs, bone levels, caries, calculus, MD, RCTs, and extensive restorative treatments. Without Restorations: − 0.42 Removing the caries component caused the most significant drop in predictive power (from -0.44 to -0.22). This makes sense clinically as caries is a common, treatable condition that often requires expensive procedures (fillings, root canals, extractions and implants). In contrast, removing other components had minimal impact. Bone loss, for example, barely affected the correlation (-0.45). Similarly, existing restorations without active disease (-0.42) typically do not need immediate treatment. This suggests that caries status is a dominant driver of near-term treatment needs and costs. Given its strong influence on predictive accuracy, future work could explore whether assigning greater weight to the caries component in the OS-B scoring system may further enhance its clinical utility. Such refinements, coupled with validation across diverse datasets, could improve the model’s ability to guide both practitioners and patients toward more timely and cost-effective interventions. OS-B scores: age and gender patterns Analysis of OS-B scores demonstrates predictable patterns across age and gender demographics. As expected, oral health scores progressively decline with age, reflecting the cumulative impact of dental diseases over time. Gender-based analysis reveals a consistent pattern where women maintain marginally higher OS-B scores compared to men across all age groups. This gender disparity aligns with established national health data, which documents men’s increased susceptibility to oral health challenges, including higher rates of periodontal disease, oral cancer, and dental trauma, often attributed to less rigorous oral hygiene practices and fewer dental visits 20 . These demographic trends in OS-B scores are visually represented in Figure 10 . Fig. 10 OS-B distribution analysis. (A) Shows the distribution of Oral Score Basic (OS-B) across four age groups: 21–40, 41–60, 61–80, and 81–100. Each age group has a violin shape representing the distribution of OS-B scores, with a mean line and 2 lines showing maximum and minimum. (B) Shows the distribution of OS-B scores for male (M) and female (F) patients. Each gender has a violin shape showing the range of OS-B scores, with a line indicating the mean and others for the maximum and minimum scores.
Overjet Frequently Asked Questions (FAQ)
When was Overjet founded?
Overjet was founded in 2018.
Where is Overjet's headquarters?
Overjet's headquarters is located at 200 State Street, Boston.
What is Overjet's latest funding round?
Overjet's latest funding round is Series C.
How much did Overjet raise?
Overjet raised a total of $130.55M.
Who are the investors of Overjet?
Investors of Overjet include Crosslink Capital, E14 Fund, Insight Partners, General Catalyst, Liquid 2 Ventures and 10 more.
Who are Overjet's competitors?
Competitors of Overjet include VideaHealth, Pearl, Adravision, KELLS, Pearlii and 7 more.
What products does Overjet offer?
Overjet's products include Insurance Intelligence Platform.
Who are Overjet's customers?
Customers of Overjet include Guardian.
Loading...
Compare Overjet to Competitors

Pearl specializes in dental artificial intelligence (AI) solutions within the healthcare technology sector. Its main offerings include an AI-enabled radiologic platform for dental diagnostics and artificial intelligence services for dental practices. Its technology is utilized by the dental industry to improve the efficiency, accuracy, and consistency of dental care. It was founded in 2019 and is based in West Hollywood, California.
VideaHealth develops artificial intelligence solutions for the dental industry. The company provides a dental artificial intelligence (AI) platform that aims to improve diagnostic accuracy and optimize practice workflows by combining clinical and workflow AI. VideaHealth targets dental service organizations (DSOs) and individual dental clinicians. VideaHealth was formerly known as DentistAI. It was founded in 2018 and is based in Boston, Massachusetts.

Denti.AI develops dental technology in the healthcare sector. The company offers products such as a dental scribe for recording clinician-patient conversations, voice-enabled perio charting for periodontal assessments, and automated X-ray diagnostics. Denti.AI primarily serves the dental healthcare industry, integrating its solutions with existing practice management systems to improve clinical workflows. It was founded in 2017 and is based in Toronto, Ontario.
Retrace is a company that provides payment solutions for the oral health care sector. It offers automation tools that assist with billing and office processes for dental practices. Retrace serves oral health care providers, payers, and patients by addressing claims processing. It was founded in 2016 and is based in San Francisco, California.
Boneprox provides digital dental care and healthcare solutions, focusing on imaging and diagnostics. The company offers services including communication platforms for telediagnostics, AI for dental imaging analysis, and education programs for dental professionals. Boneprox serves the dental and healthcare sectors with its solutions. It was founded in 2013 and is based in Gothenburg, Sweden.
Adravision provides AI-driven software solutions for dental diagnostics in the healthcare domain. The company focuses on the interpretation of dental radiographs, charting processes, and patient communication through reports. Adravision serves dental clinics, dental support organizations (DSOs), and the insurance sector. It was founded in 2021 and is based in Atlanta, Georgia.
Loading...